As American athlete Noah Lyles was wheeled off the track after securing bronze in the 200 metres at the Paris Olympics, the sheer exhaustion on his face said it all. Just moments later he revealed his Covid-19 diagnosis – he had kept it quiet beforehand so his competitors wouldn’t have the edge.
This is a supreme athlete who only days previously had secured a fantastic gold medal in the 100 metres. Now, though, he was light-headed, short of breath and suffering from chest pains. Covid symptoms that more than likely would last a relatively short period of time.

But what if they were to persist for months, if not years? Then Lyles would join the estimated 65 million people around the globe – including many formerly super-fit athletes – who have long covid. For these sufferers, whose symptoms can severely impact the quality of their daily life, the Covid-19 pandemic has never ended. Despite the amount of research invested in long covid, medical science appears far from finding a cure or pinpointing the cause of the debilitating condition.
Lingering symptoms
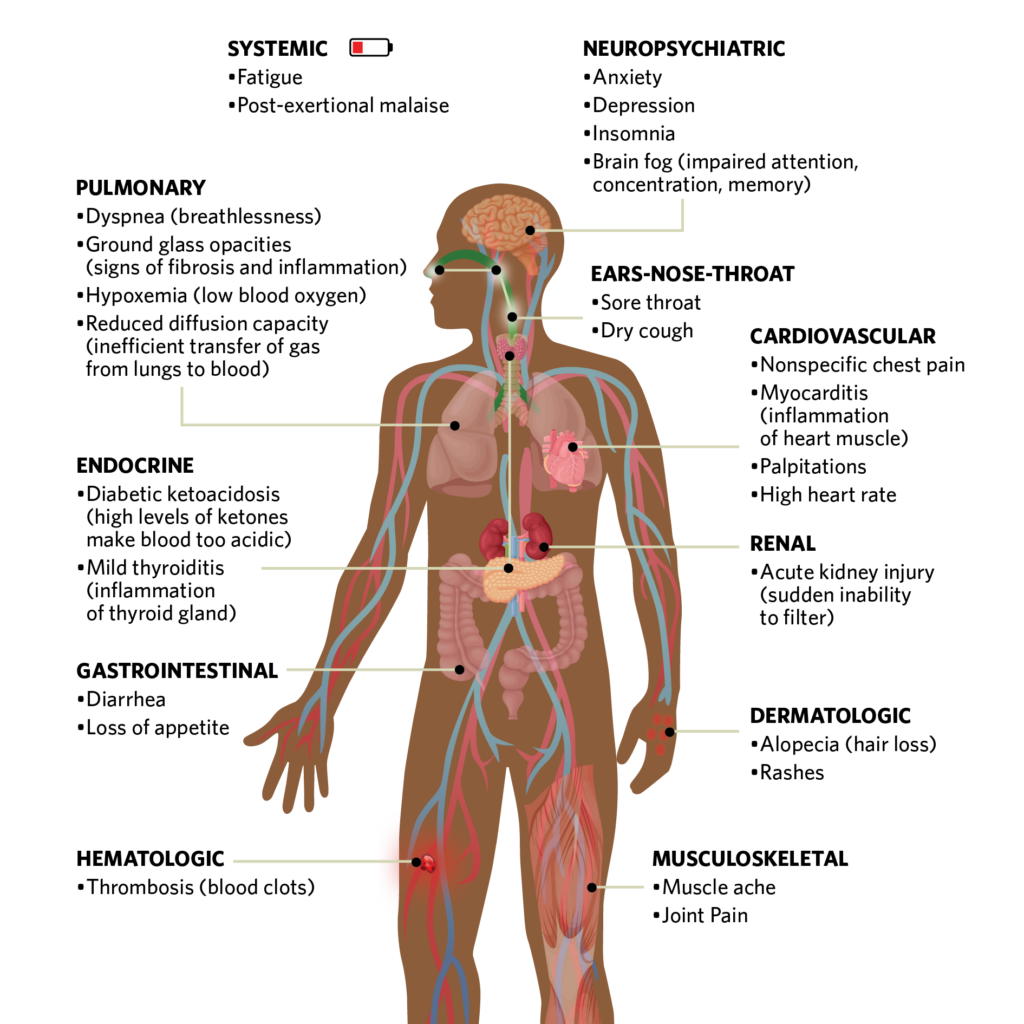
According to New Scientist, the term ‘long covid’ was used in medical circles as early as May 2020 to describe people whose covid symptoms lingered on. There are a multitude of continuing symptoms, but shortness of breath, brain fog and fatigue are most commonly cited, as well as post-exertional malaise – a feeling of exhaustion after just a short spurt of activity.
The loose consensus among the medical community is that about 10% of people infected with the SARS-CoV-2 coronavirus suffer from long covid, says David Putrino, Director of Rehabilitation Innovation at the Mount Sinai Health System in New York and an expert in the condition. The figure is the subject of continued speculation, though, and the risk of long covid appears to depend upon the viral variant. Nevertheless, some studies have predicted that up to 200 million people will develop the condition over the next decade.
The clinical definition of long covid is a persistence of Covid-19 signs and symptoms beyond four weeks; having persistent symptoms after 12 weeks that are not explained by an alternative diagnosis is deemed to be post Covid-19 syndrome – though, in practice, the two terms are often used interchangeably.
Gut action
There is no unifying theory of its cause, but rather a number of pervading theories that perhaps overlap. “One that is getting most traction is that the virus itself is hanging around in the body away from the immune system, most likely in the gut,” said David Strain, an Associate Professor at the University of Exeter Medical School, in a BBC podcast. “The virus is not getting into the blood on a regular basis, and when it does, it doesn’t get high enough to trigger any tests – [so] you aren’t going to show positive on a lateral flow test or a PCR test.”
In this situation, when sufficient virus leaks intermittently into the blood, the person re-experiences a flu-like illness and becomes exhausted for no apparent reason.
Another theory is that the infection causes a degree of permanent damage to the cell mitochondria. “The mitochondria are the powerhouse of every single cell, generating the energy you need to do any sort of activity,” says Strain. “When the virus gets into the cells, it uses the pathway that stimulates the production of mitochondria, [and doctors] are suggesting that the virus itself makes those mitochondria go dormant, which is why we run out of energy much quicker [resulting in] fatigue and brain fog.”
Capillary blockage
Micro-clotting is also being considered as a cause of long covid. As Dr Strain relates: “We know that covid causes small blood clots to form within the capillaries, the very, very small blood vessels within our body. If those small blood clots are blocking those capillaries, the body can’t get nutrients to the tissues that need them, and probably more importantly, it can’t get rid of waste products.
This would explain why some people with long covid feel fine at the start of the day, when the body has had time to replenish itself, but become exhausted very quickly soon after. “It also accounts for why people who do some exercise will take two or three days to recover – post-exertion malaise – because those toxins build up and they aren’t clearing at the normal rate,” he reveals.
Immune disruption
As reported recently in New Scientist, there is a growing body of evidence pointing to disruption in the immune system of long covid sufferers. Studies have suggested some parts of their body develop an overactive immune system, while in other parts the immune system remains underactive. Other research indicates the existence of an autoimmune disorder in which the immune system attacks the body.
Strain, however, is not so sure, since people with long covid appear to improve after receiving Covid-19 vaccinations. “If it was an autoimmune disease, the immune system ramps up [and] you may expect that vaccination to make it worse rather than better,” he notes.
Evidence that the virus persists in many parts of the body – tissues and organs, gut lining, skin and lungs – has highlighted the similarities between this and other chronic conditions such as myalgic encephalomyelitis (ME), or chronic fatigue syndrome. Strain believes it is likely that ME and long covid belong to the same family of conditions but have different underlying triggers.
Brain energy drain
Brain fog is one of the symptoms reported by sufferers of long covid. This is where people have difficulty concentrating, perhaps even struggling to get to the end of a sentence. Strain says this brain fog could stem from a lack of energy reaching the brain, though some studies suggest the virus may have caused significant brain injury.
A 2022 study in the UK involving 800,000 people explored the cognitive effects of Covid-19. On average, people who had covid for more than 12 weeks or had required hospital treatment performed worse in the cognitive tests. Even those who had symptoms for less than 12 weeks did worse than the no-confirmed-infection group. People infected early in the pandemic were shown to be among the poorest performers. This could be attributed to the effects of vaccinations and other variants coming into play.

Ultimately, many questions about the long-term consequences of Covid-19 infection on the brain remain unanswered. Separate research has suggested low levels of serotonin, a neurotransmitter, could explain cognitive symptoms that occur in long covid.
Treatment conundrum
Long covid is undoubtedly a nightmare to treat because of the huge degree of uncertainty surrounding the condition and the large number of different presentations. There is no test for long covid and it could be years of clinical trials before practitioners know how best to treat it.
Existing treatment methods include recurrent boosts of vaccines and laboratory-made antibodies to top up the immune system. Long-covid specialists advise those affected to seek a thorough assessment supplemented by a range of treatment options from psychological support to medication.